|
Housingclick to view |

|
Health Careclick to view |

|
Child Care and Educationclick to view |

|
Technologyclick to view |

|
Foodclick to view |

|
Taxesclick to view |

|
Transportationclick to view |
||
Impact on ALICE
What do families do if they cannot afford health care?
For many ALICE households, doctor visits and medications are prohibitively expensive. Low-income families face problems with the cost of care and also with access to care, including long distances to providers, language and cultural barriers, transportation challenges, difficulty navigating health care systems, and difficulty making work and child care arrangements to accommodate health care appointments.8 Because these families have limited choices for accessing the care they need, they may try to:
Go Without Regular Care
ALICE families that can’t afford health care sometimes delay or go without regular care, including preventative services (checkups, vaccinations, and screenings), dental care (exams and cleanings), and mental health services.
ALICE families that can’t afford health care sometimes delay or go without regular care, including preventative services (checkups, vaccinations, and screenings), dental care (exams and cleanings), and mental health services.
Preventative Care
Young children below the Federal Poverty Level (FPL) are less likely than those in higher-income families to receive scheduled vaccines, and low-income adults are 14 to 26 percent less likely to receive cervical, breast, and prostate cancer screenings.9
Preventative Care
Young children below the Federal Poverty Level (FPL) are less likely than those in higher-income families to receive scheduled vaccines, and low-income adults are 14 to 26 percent less likely to receive cervical, breast, and prostate cancer screenings.9

Mental Illness in Children and teens
Untreated mental illness in children and teens has severe social and educational consequences:14
- 50% - Share of children with a mental illness who received treatment in 2017
- 37% - Share of students with mental health conditions at age 14 who drop out of school
- 70% - Share of youth in the juvenile justice system who have a mental illness
Find Affordable Insurance Coverage
ALICE families often have trouble finding or affording health insurance coverage, sometimes winding up with inadequate insurance or no coverage at all
- Getting insurance through an employer is often the best option, but many lower-wage jobs where ALICE works — especially in the service industry — do not offer health insurance.15
- Lower-cost Marketplace health plans have been available since 2014 through the ACA, but the plans that ALICE families can afford often have minimal coverage and high deductibles.
- Medicaid provides free health care coverage for many households in poverty, but many ALICE families earn too much to qualify at their state’s eligibility levels.16 And some households — 2.5 million uninsured adults in non-Medicaid-expansion states — have income above current Medicaid eligibility but below the lower limit for Marketplace premium tax credits. In addition, 25 percent of those eligible for Medicaid/CHIP nationwide were still not enrolled as of 2017.17
Percent of Workers With Insurance and Employer-Sponsored Insurance, by Income, U.S., 2017
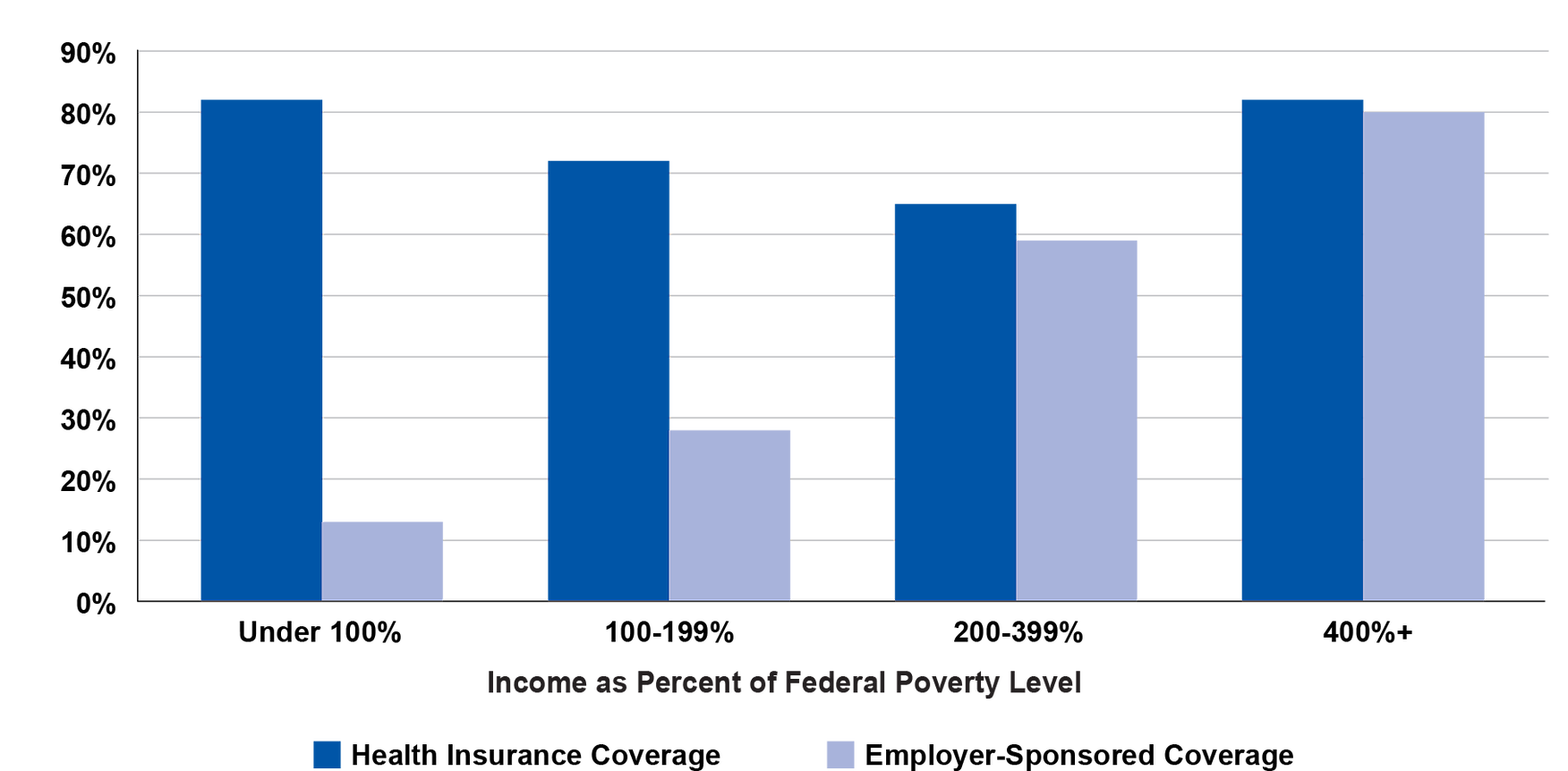
Source: Kaiser Family Foundation. (2017). State health facts: Employer-sponsored coverage rates for the nonelderly by Federal Poverty Level (FPL).
ALICE families often have trouble finding or affording health insurance coverage, sometimes winding up with inadequate insurance or no coverage at all
- Getting insurance through an employer is often the best option, but many lower-wage jobs where ALICE works — especially in the service industry — do not offer health insurance.15
- Lower-cost Marketplace health plans have been available since 2014 through the ACA, but the plans that ALICE families can afford often have minimal coverage and high deductibles.
- Medicaid provides free health care coverage for many households in poverty, but many ALICE families earn too much to qualify at their state’s eligibility levels.16 And some households — 2.5 million uninsured adults in non-Medicaid-expansion states — have income above current Medicaid eligibility but below the lower limit for Marketplace premium tax credits. In addition, 25 percent of those eligible for Medicaid/CHIP nationwide were still not enrolled as of 2017.17
Percent of Workers With Insurance and Employer-Sponsored Insurance, by Income, U.S., 2017
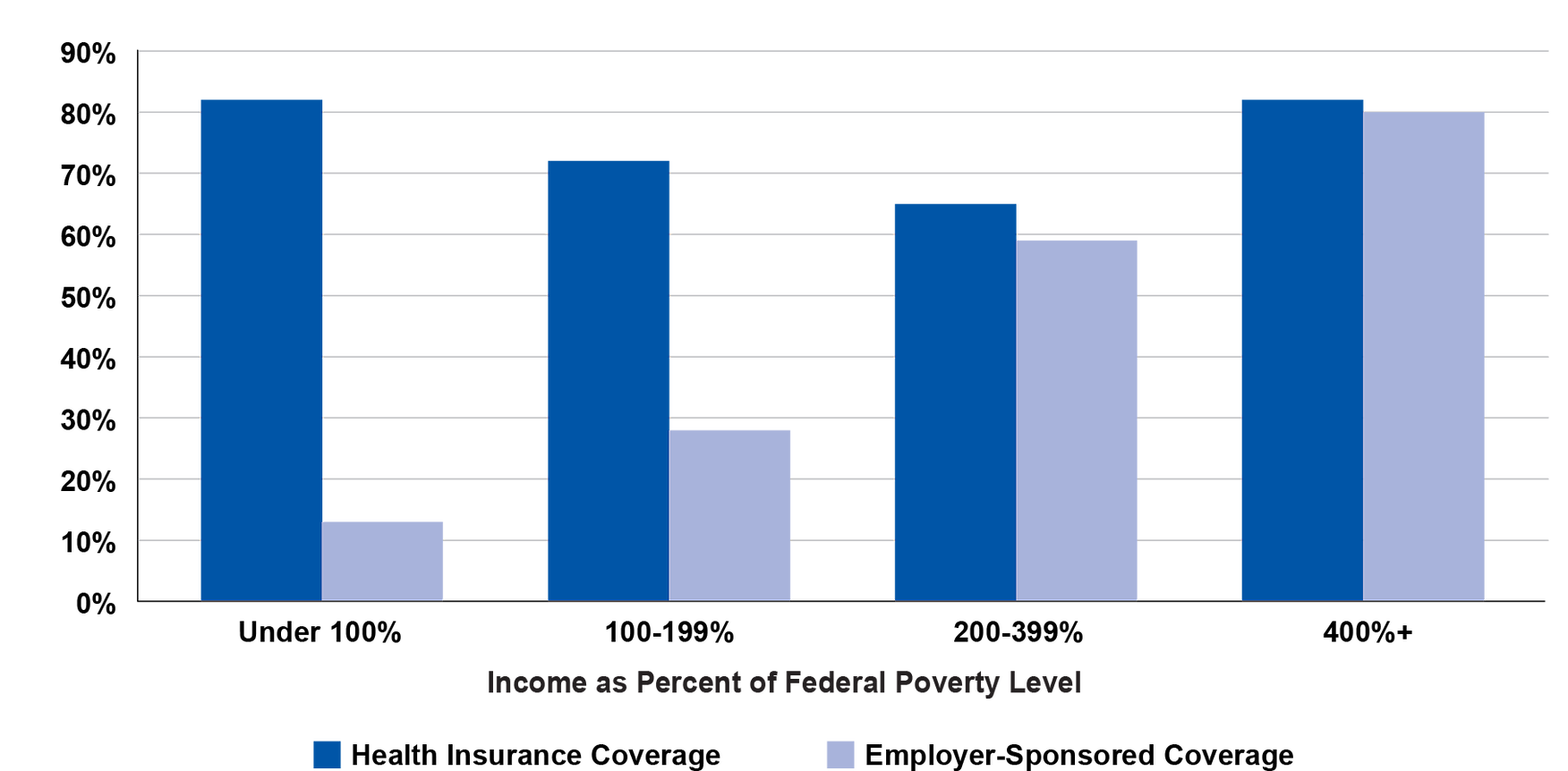
Source: Kaiser Family Foundation. (2017). State health facts: Employer-sponsored coverage rates for the nonelderly by Federal Poverty Level (FPL).

Provide Caregiving for a Family Member
Nationwide, over 40 million people provide unpaid care for a loved one who is ill, frail, or has a physical or mental disability.25 This is one way of saving money, especially given the high costs of institutions such as assisted living facilities. However, such care can end up taking a physical, mental, and financial toll on caregivers.
Nationwide, over 40 million people provide unpaid care for a loved one who is ill, frail, or has a physical or mental disability.25 This is one way of saving money, especially given the high costs of institutions such as assisted living facilities. However, such care can end up taking a physical, mental, and financial toll on caregivers.

Move to a Healthier Community
When it comes to health, where we live matters. In a large-scale study of the health of nearly 45 million people in the U.S., researchers found that over 25 percent of diseases included in the study were influenced primarily by the environment in which people live.32 Social and economic factors (like education, employment, income, and community safety); characteristics of the physical environment (including housing and air/water quality); and proximity to care all affect health outcomes.33
When it comes to health, where we live matters. In a large-scale study of the health of nearly 45 million people in the U.S., researchers found that over 25 percent of diseases included in the study were influenced primarily by the environment in which people live.32 Social and economic factors (like education, employment, income, and community safety); characteristics of the physical environment (including housing and air/water quality); and proximity to care all affect health outcomes.33

Sources
8
Kaiser Family Foundation. (2018, December 7). Key facts about the uninsured population. Retrieved from https://www.kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/
Robert Wood Johnson Foundation (2011, August 1). What is the link between having health insurance and getting adequate health care? Robert Wood Johnson Foundation. Retrieved from https://www.rwjf.org/en/library/research/2011/08/what-is-the-link-between-having-health-insurance-and-getting-ade.html
U.S. Senate Committee on Health, Education, Labor & Pensions. (2012). Dental crisis in America: The need to expand access. A Report from Chairman Bernard Sanders, Subcommittee on Primary Health & Aging. Retrieved from http://www.sanders.senate.gov/imo/media/doc/DENTALCRISIS.REPORT.pdf
9
Hill, H. A., Elam-Evans, L. D., Yankey, D., Singleton, J. A., & Kang, Y. (2017, November 3). Vaccination coverage among children aged 19–35 months, 2016. Centers for Disease Control and Prevention (CDC). Morbidity and Mortality Weekly Report (MMWR), 66(43), 1171–1177. Retrieved from https://www.cdc.gov/mmwr/volumes/66/wr/mm6643a3.htm#T2_down
Ross, J. S., Bernheim, S. M., Bradley, E. H., Teng, H.-M., & Gallo, W. T. (2007, March). Use of preventive care by the working oor in the United States. Preventive Medicine, 44(3), 254–259. Retrieved from http://www.sciencedirect.com/science/article/pii/S009174350600466X
National Health Interview Survey. (2015). Table 72. Use of colorectal tests or procedures among adults aged 50–75, by selected characteristics: United States, selected years 2000–2015. Retrieved from https://www.cdc.gov/nchs/data/hus/2017/072.pdf
10
Claxton, G., Sawyer, B., & Cox, C. (2019). How does cost affect care? Kaiser Family Foundation. Retrieved from https://www.healthsystemtracker.org/chart-collection/cost-affect-access-care/
National Health Interview Survey. (2016). Table 78. Dental visits in the past year, by selected characteristics: United States, selected years 1997–2016. Centers for Disease Control and Prevention, National Center for Health Statistics. Retrieved from https://www.cdc.gov/nchs/data/hus/2017/078.pdf
11
CDC Foundation. (2015, January 28). Worker illness and injury costs U.S. employers $225.8 billon annually. Retrieved from https://www.cdcfoundation.org/pr/2015/worker-illness-and-injury-costs-us-employers-225-billion-annually
Balfanz, R., & Byrne, V. (2012). The importance of being in school: A report on absenteeism in the nation’s public schools. Johns Hopkins University Center for Social Organization. Retrieved from http://new.every1graduates.org/wp-content/uploads/2012/05/FINALChronicAbsenteeismReport_May16.pdf
Attendance Works. (2015, September). Mapping the early attendance gap: Charting a course for student success. Retrieved from http://www.attendanceworks.org/wordpress/wp-content/uploads/2015/07/Mapping-the-Early-Attendance-Gap-Final-4.pdf
Witters, D., & Liu, D. (2013, May 7). In U.S., poor health tied to big losses for all job types. Gallup. Retrieved from http://www.gallup.com/poll/162344/poor-health-tied-big-losses-jobtypes.aspx
12
Prentice, J. C., & Pizer, S. D. (2007, April). Delayed access to health care and mortality. Health Services Research, 42(2), 644–662. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1955366/
13
U.S. Senate Committee on Health, Education, Labor & Pensions. (2012, February 29). Dental crisis in America: The need to expand access. A Report from Chairman Bernard Sanders, Subcommittee on Primary Health & Aging. Retrieved from http://www.sanders.senate.gov/imo/media/doc/DENTALCRISIS.REPORT.pdf
National Advisory Committee on Rural Health and Human Services. (2018). Improving oral health care services in rural America. U.S. Department of Health & Human Services. Retrieved from https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2018-Oral-Health-Policy-Brief.pdf
14
National Alliance on Mental Illness (NAMI). (2019). Mental illness. Retrieved from https://www.nimh.nih.gov/health/statistics/mental-illness.shtml
15
An, J., Braveman, P., Dekker, M., Egerter, S., & Grossman-Kahn, R. (2011). Work, workplaces and health. Robert Wood Johnson Foundation. Retrieved from https://www.rwjf.org/en/library/research/2011/05/work-and-health-.html
Lynch, J., Smith, G.D., Harper, S., & Hillemeier, M. (2004). Is income inequality a determinant of population health? Part 2. U.S. National and regional trends in income inequality and age- and cause-specific mortality. Milbank Quarterly, 82(2), 355–400. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15225332
Greenwald, L. & Fronstin, P. (2019). The state of employee benefits: Findings from the 2018 health and workplace benefits survey, (Issue Brief No. 470). Employee Benefit Research Institute. Retrieved from https://www.ebri.org/docs/default-source/ebri-issue-brief/ebri_ib_470_wbs2-10jan19.pdf?sfvrsn=c5db3e2f_2
Kaiser Family Foundation (2019). Distribution of the nonelderly with employer coverage by Federal Poverty Level (FPL). Retrieved from https://www.kff.org/private-insurance/state-indicator/distribution-by-fpl-3/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
16
Kaiser Family Foundation. (2019, May 13). Status of state action on the Medicaid expansion decision. Retrieved from https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
17
Kaiser Family Foundation. (2017). Distribution of eligibility for ACA health coverage among those remaining uninsured as of 2017. Retrieved from https://www.kff.org/health-reform/state-indicator/distribution-of-eligibility-for-aca-coverage-among-the-remaining-uninsured/?currentTimeframe=0&selectedDistributions=medicaidother-public-eligible&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
18
DeLia, D., & Lloyd, K. (2014, July). Sources of variation in avoidable hospital use and cost across low-income communities in New Jersey. Rutgers Center for State Health Policy. Retrieved from http://www.cshp.rutgers.edu/downloads/10470.pdf
Dolan, R. (2016, February 4). Health policy brief. Robert Wood Johnson Foundation. Retrieved from http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_152.pdf
19
Altman, D. (2019, April 15). For low-income people, employer health coverage is worse than ACA. Kaiser Family Foundation. Retrieved from https://www.kff.org/health-costs/perspective/for-low-income-people-employer-health-coverage-is-worse-than-aca/
20
Collins, S. R., Bhupal, H. K., & Doty, M. M. (2019). Health insurance coverage eight years after the ACA: Fewer uninsured Americans and shorter coverage gaps, but more underinsured. The Commonwealth Fund. Retrieved from https://www.commonwealthfund.org/sites/default/files/2019-02/Collins_hlt_ins_coverage_8_years_after_ACA_2018_biennial_survey_sb.pdf
21
The Commonwealth Fund. (2015, November 20). How high Is America’s health care cost burden? Retrieved from http://www.commonwealthfund.org/publications/issue-briefs/2015/nov/how-high-health-care-burden
Pollitz, K., Cox, C., Lucia, K., & Keith, K. (2014, January 7). Medical debt among people with health insurance. Kaiser Family Foundaiton. Retrieved from https://www.kff.org/private-insurance/report/medical-debt-among-people-with-health-insurance/
McElwee, S. (2016). Enough to make you sick: The burden of medical debt. Demos. Retrieved from http://www.demos.org/publication/enough-make-you-sick-burden-medical-debt
Richard, P., Walker, R., & Alexandre, P. (2018). The burden of out of pocket costs and medical debt faced by households with chronic health conditions in the United States. PLOS ONE, 13(6), e0199598. Retrieved from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0199598
22
Dague, L., DeLeire, T., & Leininger, L. (2014). The effect of Public insurance coverage for childless adults on labor supply (Working Paper No. 20111). National Bureau of Economic Research. Retrieved from http://www.nber.org/papers/w20111.pdf
Sloan, F., & Hsieh, C.-R. (2017). Health economics (2nd ed.). Retrieved from https://mitpress.mit.edu/books/health-economics-second-edition
23
Collins, S. R., Bhupal, H. K., & Doty, M. M. (2019). Health insurance coverage eight years after the ACA: Fewer uninsured Americans and shorter coverage gaps, but more underinsured. The Commonwealth Fund. Retrieved from https://www.commonwealthfund.org/sites/default/files/2019-02/Collins_hlt_ins_coverage_8_years_after_ACA_2018_biennial_survey_sb.pdf
24
National Association of Dental Plans. (2016). Who has dental benefits today? Retrieved from http://www.nadp.org/Dental_Benefits_Basics/Dental_BB_1.aspx
Medicare. (2016). Your Medicare coverage: Eye exams. Retrieved from https://www.medicare.gov/coverage/eye-exams.html
25
Bonner, A. (2015, March). 2015 AARP National Caregiving Survey of Registered Voters Age 40 and Older. AARP. Retrieved from https://www.aarp.org/research/topics/care/info-2015/national-survey-family-caregivers.html
26
AARP Public Policy Institute. (2015). Caregiving in the U.S. 2015. National Alliance for Caregiving. Retrieved from http://www.caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Final-Report-June-4_WEB.pdf
27
Rainville, C., Skufca, L., & Mehegan, L. (2016). Family Caregivers Cost Survey: What they spend & what they sacrifice. AARP. Retrieved from https://www.aarp.org/research/topics/care/info-2016/family-caregivers-cost-survey.html
28
Rainville, C., Skufca, L., & Mehegan, L. (2016). Family Caregivers Cost Survey: What they spend & what they sacrifice. AARP. Retrieved from https://www.aarp.org/research/topics/care/info-2016/family-caregivers-cost-survey.html
29
AARP Public Policy Institute. (2015). Caregiving in the U.S. 2015. National Alliance for Caregiving. Retrieved from http://www.caregiving.org/wp-content/uploads/2015/05/2015_CaregivingintheUS_Final-Report-June-4_WEB.pdf
30
MetLife Mature Market Institute. (2010, February). The MetLife study of working caregivers and employer health care costs. Retrieved from https://nrrs.ne.gov/respite/employers/docs/metlife_working-caregivers-employers-health-care-costs.pdf
31
Leventhal, T. & Brooks-Gunn, J. (2003). Moving to opportunity: An experimental study of neighborhood effects on mental health. American Journal of Public Health, 93(9), 1576–1582. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1448013/
32
Pesheva, E. (2019). ZIP code or genetic code? Harvard Medical School. Retrieved from https://hms.harvard.edu/news/zip-code-or-genetic-code
33
Bachrach, D., Pfister, H., Wallis, K., & Lipson, M. (2014). Addressing patients’ social needs. The Commonwealth Fund. Retrieved from http://www.commonwealthfund.org/~/media/files/publications/fund-report/2014/may/1749_bachrach_addressing_patients_social_needs_v2.pdf
Robert Wood Johnson Foundation. (2011, December 1). Health care’s blind side: The overlooked connection between social needs and good health: Summary of findings from a survey of America’s physicians. Retrieved from http://www.rwjf.org/files/research/RWJFPhysiciansSurveyExecutiveSummary.pdf
Levi, J., Segal, L.M., & Kohn, D. (2015, June 17). The facts hurt — a state-by-state injury prevention policy report. Trust for America’s Health. Retrieved from https://www.tfah.org/releases/injuryprevention15/
Egerter, S., Barclay, C., Grossman-Kahn, R., & Braveman. P. (2011). Violence, social disadvantage, and health (Issue Brief No. 10). Robert Wood Johnson Foundation. Retrieved from http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.654.3851&rep=rep1&type=pdf
Robert Wood Johnson Foundation. (2012, October 25). How does transportation impact health? Retrieved from https://www.rwjf.org/en/library/research/2012/10/how-does-transportation-impact-health-.html
Clark, L. P., Millet, D. B., & Marshall, J. D. (2014, April 15). National patterns in environmental injustice and inequality: Outdoor NO2 air pollution in the United States. PLOS ONE. Retrieved from http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0094431
VanDerslice, J. (2011). Drinking water infrastructure and environmental disparities: Evidence and methodological considerations. American Journal of Public Health, 101(Supplement 1), 109–114. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222486/
34
University of Wisconsin Population Health Institute. (2019). What works for health. Retrieved from http://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health
35
Hall, M., Crowder, K., & Spring, A. (2015, April 21). Neighborhood foreclosures, racial/ethnic transitions, and residential segregation. American Sociological Review, 80(3), 526–549. Retrieved from https://doi.org/10.1177/0003122415581334
Urban Institute. (n.d.). Exposing housing discrimination. Retrieved from https://www.urban.org/features/exposing-housing-discrimination
36
Egerter, S., Braveman, P., & Barclay, C. (2011). Stress and health. Robert Wood Johnson Foundation. Retrieved from https://www.rwjf.org/en/library/research/2011/03/how-social-factors-shape-health.html
House, J. S. (2001, March-April). Social isolation kills, but how and why? Psychosomatic Medicine, 63(2), 273–274. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11292275